Abstract
Introduction;
Polycythemia Vera (PV), is one of the most common Philadelphia chromosome negative myeloproliferative disorders. The identification of Janus Kinase (JAK) 2 mutations and the publication of 2016 revision of WHO classification of myeloid neoplasms has improved diagnostic accuracy of PV. The lower cut-off values of Hemoglobin (Hb) and hematocrit (Hct) used in WHO diagnostic criteria, however, resulted in increased number of adult patients undergoing further evaluation for PV leading to identification of patients with acquired, idiopathic Persistent polycythemia (PP) who not meet WHO criteria for PV despite extensive work up. The clinicopathologic features, disease course, treatment and outcomes of these patients has not been well characterize. This study seeks to described clinicopathologic and molecular profile of cohort of adult patients with Non Hereditary, Non-Polycythemia Vera (NHNPV) Persistent Polycythemia.
Methodology;
Patients with PP diagnosed and followed up in Fresno community regional medical center/University of San Francisco (UCSF) Fresno, from January 2010 to December 2020 were reviewed. Patients who didn't meet WHO diagnostic criteria for PV after full evaluation including bone marrow biopsies were included in the study. Those with incomplete evaluation, clearly attributable secondary causes of polycythemia or erythropoietin (EPO) level above institutional laboratory reference range (2-18), were excluded from the study. Patients with polycythemia diagnosed at pediatric age were also excluded. The study was approved by institutional review board of UCSF Fresno.
Results;
129 subjects with JAK 2 Negative PP were reviewed of which 63 had EPO levels within or below the normal range (2-18).
Of 36 patients who met the study inclusion and exclusion criteria, majority were males (70% N= 28) and non-Hispanic (56% N=20) with median age at diagnosis of 48.5 years (range 18-70 years). Half of the patients (N=18) have no identifiable etiology of PP. In patients with associated conditions, the most common is non-oxygen requiring clinical OSA (36%) and tobacco smoking (19.4%). Of note, all these patients have EPO level less than 10 which represents the median value of the local institutional defined normal range for EPO. Four (11%) patients have non-iron overloaded hemochromatosis gene mutation (1 Homozygous H63D HFE gene, 2 heterozygous mutation and one with unspecified mutation type).
Average Hb and Hct at diagnosis was (17.26+/- 2.23) and (49.76+/- 6.34) respectively. Mean EPO level 7.05+/-2.75 with less than third of patients 8 (22%) with level less or equal to in 5 units. There is no statistically significance difference between mean diagnostic EPO level between males and females in the study (7.20+/-2.89 vs.6.51+/-2.26) and so is the Hct though males have numerically higher levels.
The most common bone marrow morphology includes normocellularity (51.76+/-10.36) with erythroid hyperplasia (25%) or megakaryocyte hyperplasia without dysplasia (17%) and grade 1/3 fibrosis 6/36.
Abnormal mutations were identified in 17 patients whose bone marrow biopsies were evaluated with limited or extensive next generation sequencing (NGS). Of those patients with available results, 6 patients (35% out of those with NGS) have identifiable previously well described genetic mutations {FANCA S1311fs*1, HGF R134H, TP53 splice site 97-2A>G, KMT2A (Gain), MLL3 (KMT2C) and AFF4, ASXL1 c.1934dupG/TrpfsX12 (p. Gly646)}.
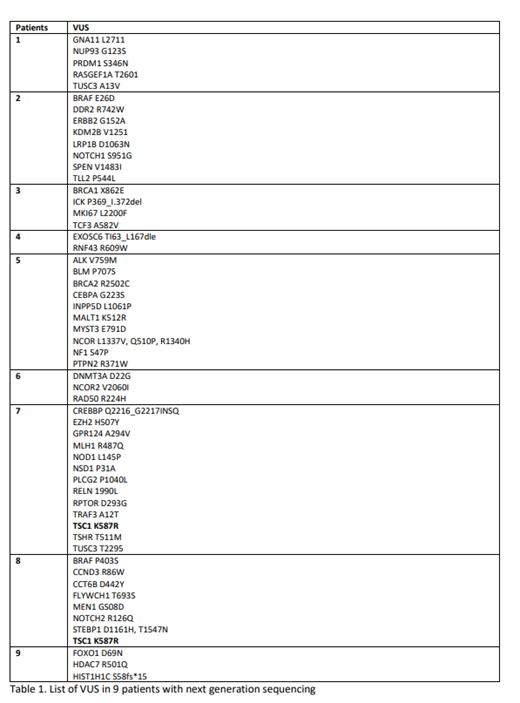
9 patients had variance of unknown significant (VUS) mutations (Table 1) with average of 6.2 mutation per patient. Only 1 VUS (TSC1 K587R) was reported in 2 different patients (#7, #9)
Mild Myeloproliferative neoplasia (MPN) associated symptoms was reported in 22% of patient with Intermittent phlebotomy (72% N= 26) and aspirin (75% N=27) was the treatment for majority of patients. One patient died during the follow up period. No patient progressed to other MPN, myelofibrosis or AML during the study period.
Conclusion;
With improved diagnostic criteria and accuracy of PV, increased number of patients are diagnosed with NHNPV Persistent polycythemia. None of the mutation or VUS identified from extensive evaluation is recurrent in our cohort of patient. Longer follow up is needed to delineate clinical significance and prognosis of these mutation in patients with NHNPV persistent Polycythemia.
Abdulhaq: BMS, Alexion, Oncopeptides, Morphosys, Pfizer, Norvartis: Honoraria; Oncopeptides, Alexion, Amgen: Speakers Bureau; Morphosys, BMS, Amgen: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal